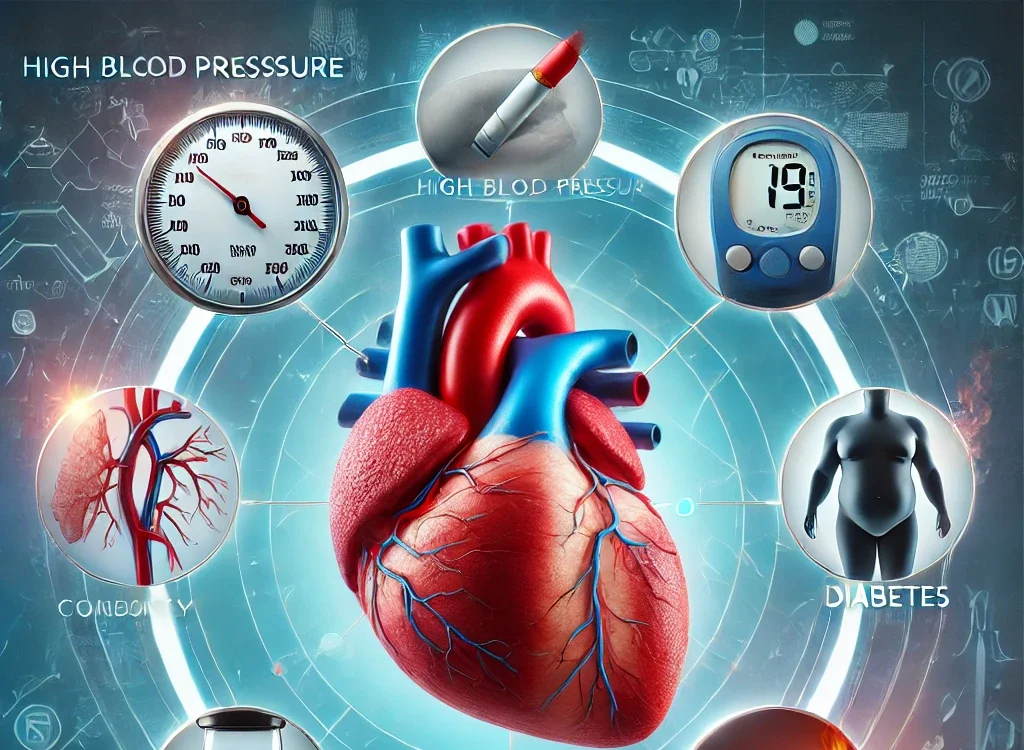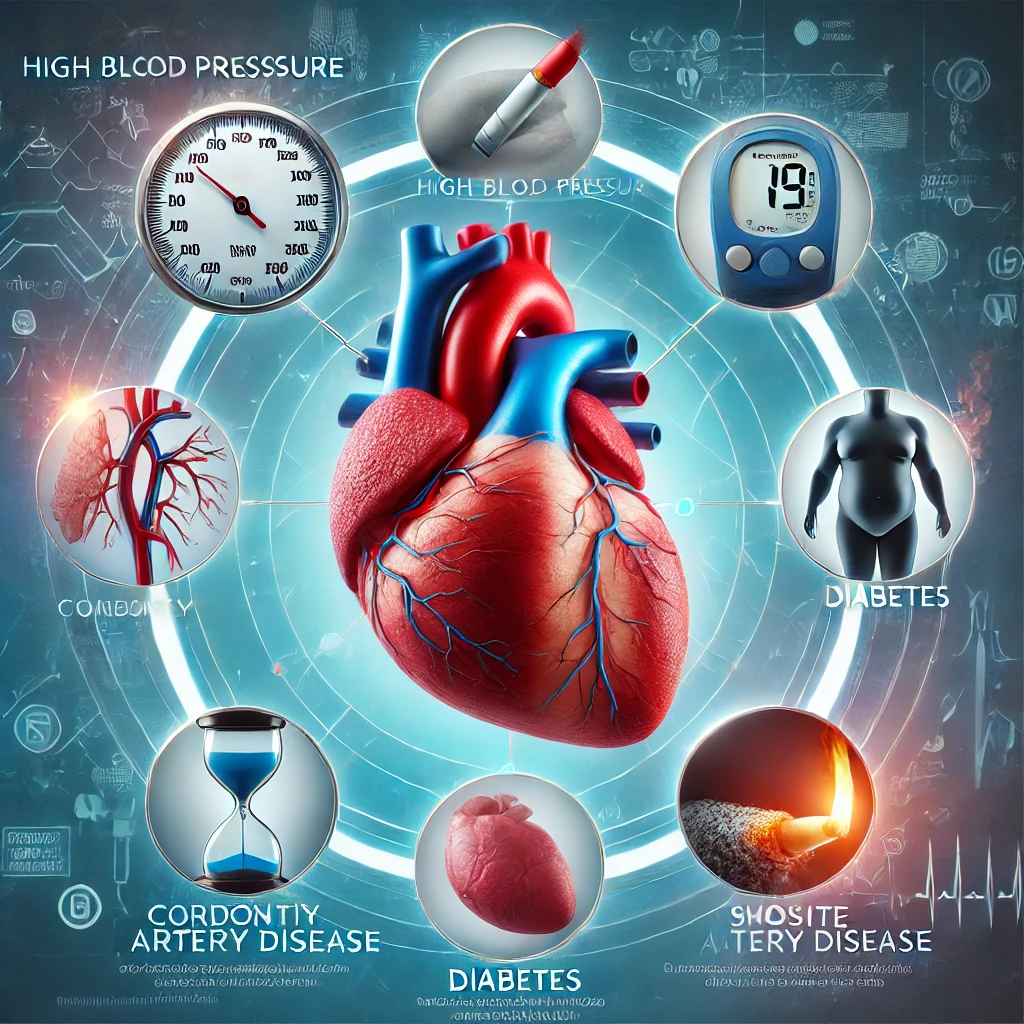
Heart failure occurs when the heart cannot pump blood efficiently enough to meet the body’s needs. This condition can develop over time, often due to factors and underlying diseases. Below are the detailed reasons that can lead to heart failure:
1. Coronary Artery Disease (CAD)
- Mechanism: Coronary artery disease (CAD) is the most common cause of heart failure. It occurs when the coronary arteries (the blood vessels that supply oxygen-rich blood to the heart) become narrowed or blocked due to plaque buildup (atherosclerosis). This reduces blood flow to the heart muscle, resulting in oxygen deprivation.
- Impact: When the heart muscle doesn’t get enough oxygen, it can become weak and less able to pump blood effectively. Over time, this can lead to heart failure.
- Progression: If CAD causes a heart attack (myocardial infarction), the heart muscle may be permanently damaged, further decreasing its pumping capacity.
Top 25 Common Workout Myths Debunked: What You Need to Know for Effective Fitness
2. High Blood Pressure (Hypertension)
- Mechanism: Chronic high blood pressure forces the heart to pump against greater resistance. This increased workload causes the heart’s left ventricle (the main pumping chamber) to become thicker and stiffer over time—a condition called left ventricular hypertrophy.
- Impact: As the ventricle thickens, it may become less able to relax and fill with blood properly, reducing the amount of blood the heart can pump. If left untreated, this can lead to heart failure.
- Progression: Untreated hypertension can also contribute to other issues like CAD, further increasing the risk of heart failure.
3. Heart Attack (Myocardial Infarction)
- Mechanism: A heart attack occurs when a blood clot blocks a coronary artery, causing a sudden loss of blood flow to part of the heart muscle. This results in tissue damage and the death of heart muscle cells.
- Impact: The area of the heart muscle that dies cannot pump blood, weakening the heart’s overall ability to function. After a heart attack, scar tissue replaces the damaged muscle, which doesn’t contract, reducing the heart’s efficiency.
- Progression: Over time, the heart muscle’s ability to pump effectively declines, leading to heart failure, particularly if there is a large area of damage.
4. Cardiomyopathy
- Mechanism: Cardiomyopathy refers to diseases of the heart muscle that can cause it to become enlarged, thickened, or stiffened. There are different types of cardiomyopathy:
- Dilated Cardiomyopathy: The heart chambers enlarge and weaken, reducing pumping capacity.
- Hypertrophic Cardiomyopathy: The heart muscle thickens, obstructing blood flow and making the heart unable to pump effectively.
- Restrictive Cardiomyopathy: The heart’s walls become rigid, restricting the heart’s ability to expand and fill with blood properly.
- Impact: The heart’s ability to pump blood diminishes, leading to fluid buildup in the body, characteristic of heart failure.
- Causes: Cardiomyopathy can be caused by genetic factors, alcohol abuse, viral infections, certain medications, or other underlying conditions.
Effective Strategies to Control the Greenhouse Effect: Mitigating Climate Change and its Impact
5. Heart Valve Disease
- Mechanism: The heart has four valves that help regulate blood flow through its chambers. If these valves become damaged, they can cause blood to leak backwards (regurgitation) or obstruct blood flow (stenosis). This puts added pressure on the heart.
- Impact: The heart works harder to compensate for the malfunctioning valves, eventually leading to the heart’s enlargement and weakening its ability to pump blood effectively.
- Progression: Chronic valve problems can lead to heart failure if the strain on the heart continues for years.
6. Arrhythmias (Irregular Heartbeats)
- Mechanism: Arrhythmias, such as atrial fibrillation or ventricular tachycardia, are abnormal heart rhythms that disrupt the heart’s ability to beat in a coordinated manner. This can lead to either an excessively fast or slow heart rate.
- Impact: Irregular heartbeats reduce the heart’s efficiency, meaning it can’t pump enough blood to meet the body’s needs. In cases like atrial fibrillation, blood may pool in the heart’s chambers, increasing the risk of clot formation.
- Progression: Chronic arrhythmias can cause structural changes to the heart and weaken the heart muscle, leading to heart failure.
7. Congenital Heart Defects
- Mechanism: Some people are born with heart defects, such as holes in the heart (septal defects), abnormal heart valves, or malformations of the heart’s structure. These defects can interfere with normal blood flow and strain the heart.
- Impact: If the heart cannot function properly due to these defects, it can lead to heart failure as it works harder to maintain blood circulation.
- Progression: Over time, the heart muscle may weaken, resulting in heart failure.
8. Chronic Kidney Disease
- Mechanism: The kidneys and heart are closely connected. When the kidneys fail, they can cause fluid and waste to build up in the body. The kidneys also help regulate blood pressure, and if they are not functioning well, this can lead to high blood pressure, which further stresses the heart.
- Impact: The excess fluid makes the heart work harder to pump blood, leading to heart failure. Moreover, kidney disease can worsen heart failure by causing fluid retention.
- Progression: If both the heart and kidneys are affected, it creates a vicious cycle where each condition worsens the other.
9. Diabetes
- Mechanism: Diabetes leads to high blood sugar levels, which can damage blood vessels and the heart muscle over time. The condition also increases the risk of high blood pressure, high cholesterol, and coronary artery disease, all of which are risk factors for heart failure.
- Impact: Damage to the heart’s blood vessels and the thickening of the heart muscle due to high blood sugar can reduce the heart’s pumping ability, leading to heart failure.
- Progression: Poorly controlled diabetes accelerates the development of heart disease, making heart failure more likely.
10. Excessive Alcohol or Drug Use
- Mechanism: Chronic alcohol abuse can lead to a condition known as alcoholic cardiomyopathy, in which the heart muscle becomes weakened and enlarged. Drugs like cocaine and methamphetamines can also cause heart damage and arrhythmias, leading to heart failure.
- Impact: These substances damage the heart muscle, disrupt the heart’s rhythm and contribute to other risk factors like high blood pressure.
- Progression: Long-term abuse of alcohol or drugs can lead to chronic heart failure, especially if combined with other risk factors.
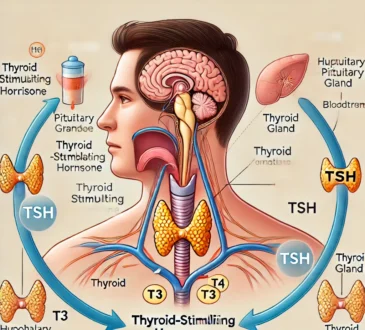
11. Thyroid Disorders
- Mechanism: Both an overactive thyroid (hyperthyroidism) and an underactive thyroid (hypothyroidism) can affect the heart. Hyperthyroidism causes an increase in heart rate and workload, while hypothyroidism can lead to a slow heart rate and fluid retention.
- Impact: An overactive thyroid increases the heart’s demand for oxygen, while an underactive thyroid can slow the heart’s pumping efficiency. Both conditions can lead to heart failure if untreated.
- Progression: Thyroid disorders can disrupt the balance of heart function, contributing to heart failure.
12. Sleep Apnea
- Mechanism: Sleep apnea is characterized by repeated episodes of stopped breathing during sleep, which leads to oxygen deprivation and increased strain on the heart. The heart works harder to compensate for low oxygen levels, causing elevated blood pressure and heart enlargement.
- Impact: Untreated sleep apnea increases the risk of arrhythmias, high blood pressure, and heart failure.
- Progression: Chronic sleep apnea can lead to worsening heart failure due to the increased strain on the cardiovascular system.
13. Infections (e.g., Myocarditis)
- Mechanism: Infections such as viral myocarditis cause inflammation of the heart muscle, which can damage the heart tissue. Other infections, like endocarditis (infection of the heart valves), can also contribute to heart failure.
- Impact: The inflammation caused by infection weakens the heart muscle, impeding its ability to pump blood.
- Progression: If the infection causes lasting damage to the heart muscle, it can lead to chronic heart failure.
14. Nutritional Deficiencies
- Mechanism: Severe deficiencies in certain nutrients, such as thiamine (vitamin B1), can lead to a condition called beriberi, which affects the heart and can lead to heart failure.
- Impact: Inadequate nutrition weakens the heart muscle, making it less able to pump effectively.
- Progression: Chronic malnutrition or deficiency can contribute to heart failure, particularly in people with other risk factors.
15. Age
- Mechanism: As we age, the heart naturally becomes less efficient. The heart muscle may stiffen, and the valves can become less effective at regulating blood flow. Additionally, the coronary arteries may become narrower.
- Impact: These age-related changes reduce the heart’s ability to pump blood effectively, increasing the risk of heart failure.
- Progression: Age-related decline in heart function can eventually lead to heart failure, particularly if other risk factors are present.
16. Chronic Lung Diseases (e.g., Chronic Obstructive Pulmonary Disease – COPD)
- Mechanism: Chronic lung diseases, especially COPD, can place a significant strain on the heart. These conditions reduce the oxygen levels in the blood, making the heart work harder to supply oxygen to the body. Over time, this extra burden on the right side of the heart can lead to a form of heart failure known as “cor pulmonale.”
- Impact: In cor pulmonale, the right side of the heart becomes enlarged and weakened due to the increased effort needed to pump blood through the lungs. This can lead to heart failure, particularly when the lungs and heart work inefficiently.
- Progression: As lung function deteriorates, the heart’s ability to pump blood effectively diminishes, and this can lead to systemic fluid retention and eventual heart failure.
17. Obesity
- Mechanism: Obesity increases the risk of developing conditions like high blood pressure, diabetes, and coronary artery disease, all of which can lead to heart failure. Additionally, the increased body fat can make the heart work harder to supply blood to the body.
- Impact: Obesity contributes to an increase in the size of the heart (particularly the left ventricle) and can cause the heart to become stiff, leading to difficulty filling with blood properly. This condition, known as “diastolic heart failure,” is often seen in obese individuals.
- Progression: The added strain on the heart from excess weight over time can lead to long-term damage and heart failure. Obesity is also associated with sleep apnea, which further exacerbates heart failure risk.
18. Alcoholic Cardiomyopathy
- Mechanism: Chronic heavy drinking or alcohol abuse is a direct cause of cardiomyopathy, a disease of the heart muscle. Alcohol can weaken the heart muscle, leading to dilated cardiomyopathy where the heart chambers become enlarged and unable to pump blood efficiently.
- Impact: Alcohol can interfere with the heart’s ability to contract, reducing its ability to pump blood to vital organs. Additionally, alcohol increases the risk of high blood pressure and arrhythmias, which can further damage the heart.
- Progression: With continued heavy drinking, the condition worsens, often leading to severe heart failure. In some cases, stopping alcohol consumption may improve the heart’s function, but significant damage may already be done.
19. Pregnancy-Related Complications (e.g., Peripartum Cardiomyopathy)
- Mechanism: Peripartum cardiomyopathy is a rare form of heart failure that occurs during the last month of pregnancy or within five months after childbirth. It is thought to be related to the stress of pregnancy on the cardiovascular system and, in some cases, genetic factors.
- Impact: The condition weakens the heart’s ability to pump blood effectively, leading to fluid buildup in the lungs and other parts of the body. In some cases, it may resolve after childbirth, but in others, it can progress to chronic heart failure.
- Progression: While some women recover fully from peripartum cardiomyopathy, others may continue to experience heart problems, including persistent heart failure.
20. Chemotherapy and Radiation Therapy
- Mechanism: Certain cancer treatments, particularly chemotherapy drugs like doxorubicin and trastuzumab, can damage the heart muscle. Radiation therapy targeted at the chest area can also lead to heart damage by causing inflammation of the heart tissue.
- Impact: These treatments can directly cause cardiomyopathy and lead to both acute and chronic heart failure, depending on the dosage and length of treatment. The risk of heart failure increases when chemotherapy and radiation are combined with other preexisting conditions like high blood pressure.
- Progression: Heart failure from cancer treatment can develop years after treatment ends, and it may be long-lasting or progressive.
21. Chronic Inflammation and Autoimmune Diseases
- Mechanism: Chronic inflammation, often seen in autoimmune diseases like lupus, rheumatoid arthritis, and scleroderma, can damage the heart tissue and lead to heart failure. These conditions can cause inflammation in the heart itself (myocarditis) or in the blood vessels (vasculitis), both of which affect heart function.
- Impact: The inflammation leads to scarring and thickening of the heart muscle, which weakens its ability to pump blood. This can cause fluid retention and heart failure symptoms.
- Progression: Over time, uncontrolled inflammation can progressively damage the heart muscle, leading to chronic heart failure.
22. Increased Blood Sugar (Hyperglycemia)
- Mechanism: Prolonged high blood sugar levels, even in those who are not diabetic, can damage the blood vessels and contribute to heart disease. Hyperglycemia accelerates the buildup of plaque in the arteries, which can lead to coronary artery disease and eventually heart failure.
- Impact: The damaged blood vessels reduce the heart’s ability to receive oxygen-rich blood, weakening the heart muscle and increasing the risk of heart failure.
- Progression: If high blood sugar levels are not controlled, they can contribute to long-term damage to the heart, leading to progressive heart failure.
23. Chronic Stress and Mental Health Disorders
- Mechanism: Chronic stress, depression, and anxiety can negatively affect heart health. Stress hormones, like cortisol and adrenaline, can increase heart rate and blood pressure, putting extra strain on the heart. Long-term mental health issues also contribute to behaviours like poor diet, lack of exercise, and substance abuse, which can all increase the risk of heart failure.
- Impact: Elevated stress hormones can lead to arrhythmias, high blood pressure, and inflammation, all of which contribute to heart failure.
- Progression: Chronic stress and poor mental health often contribute to a cycle of physical and emotional tolls on the heart, worsening the progression of heart failure.
24. Dehydration and Electrolyte Imbalance
- Mechanism: Severe dehydration and electrolyte imbalances (e.g., low potassium or magnesium levels) can disrupt the heart’s electrical system, leading to arrhythmias. In extreme cases, dehydration can cause the heart to stop beating.
- Impact: Persistent dehydration can cause the heart to work harder to pump blood, leading to fluid retention and eventually heart failure.
- Progression: Dehydration combined with electrolyte imbalances can lead to further strain on the heart, contributing to worsening heart failure if not corrected.
25. Smoking
- Mechanism: Smoking is a major risk factor for coronary artery disease, as it contributes to the buildup of plaque in the arteries. It also increases blood pressure and the risk of blood clots, both of which can contribute to heart failure.
- Impact: The toxic chemicals in cigarettes damage the heart and blood vessels, leading to atherosclerosis, arrhythmias, and weakened heart function. Smoking can also exacerbate other conditions like high blood pressure and diabetes, further increasing heart failure risk.
- Progression: Long-term smoking increases the risk of heart failure significantly, and the damage can worsen if smoking continues.
26. Sedentary Lifestyle
- Mechanism: Lack of physical activity is a significant risk factor for heart failure. Inactivity contributes to obesity, high blood pressure, and diabetes, which are all major contributors to heart disease and heart failure.
- Impact: A sedentary lifestyle leads to weakened muscles, including the heart muscle, and can reduce the heart’s ability to pump efficiently.
- Progression: Over time, inactivity can contribute to the development of heart failure, especially when combined with other risk factors like poor diet or obesity.
27. Fluid Retention
- Mechanism: Fluid retention can result from various causes, including kidney disease, excessive salt intake, or heart valve problems. When fluid builds up in the body, the heart is forced to pump harder to circulate it.
- Impact: The extra fluid puts strain on the heart and can lead to heart failure symptoms such as swelling in the legs and ankles, shortness of breath, and fatigue.
- Progression: If fluid retention is left untreated, it can worsen heart failure by further taxing the heart’s ability to pump blood efficiently.
Conclusion:
Heart failure can result from a variety of underlying conditions, each contributing to the weakening of the heart muscle or disruption of its pumping function. Managing risk factors such as high blood pressure, diabetes, and coronary artery disease is crucial in preventing or slowing the progression of heart failure. Treatment can include lifestyle changes, medications, medical procedures, and in some cases, surgery to correct underlying issues.